Index for Continuing Professional Development Essentials
Click teal headings to move to that section
Interprofessional Collaborative Education
Evidence in Support of Interprofessional Collaborative Education
Supported Activity Types & Credit Types
Benefits of Partnering with CPD
CPD Vision & Mission
- Vision Statement: Facilitation of optimal patient outcomes through an organizational commitment to lifelong learning of medical professionals, collaborative education to enhance team performance, and the equitable development of all team members.
- Mission: The Continuing Professional Development (CPD) program exists to further the values & commitment of Sutter Health’s mission to enhance the well-being of people in the communities we serve through a commitment to compassion & excellence in healthcare. We achieve this by advancing Interprofessional Collaborative Education (IPCE) to improve the performance of the TEAM.
(What is) Interprofessional Collaborative Education
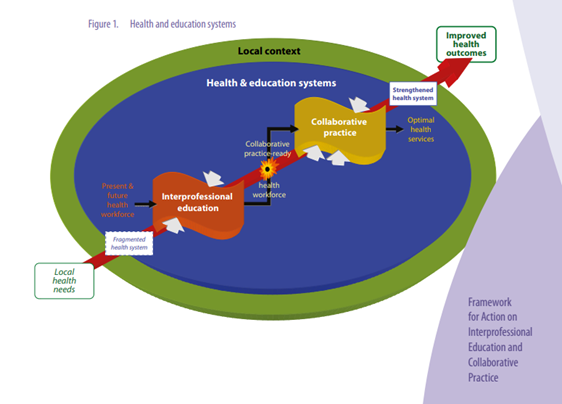
- “Interprofessional Collaborative Education (IPCE) refers to occasions when two or more professionals learn with, from, and about each other to improve collaboration and the quality of care.
- This contrasts with silo education for single disciplines or multi-professional education where health professionals learn alongside one another in a parallel manner.
- Several studies have shown that IPCE promotes interdisciplinary collaboration and teamwork, reduces the barriers and preconceptions prevailing among various healthcare groups and promotes professional competencies.
- This approach of engaging multiple health workers from different professional backgrounds working together with patients, families and communities has been shown to provide the highest quality of patient care.”
- Sources: (1) The effectiveness of interprofessional education in healthcare: A systematic review and meta-analysis (Guraya & Barr, 2017) & (2) Definition of Interprofessional Collaborative Education (ACCME, ACPE, ANCC< 2015).
Evidence in Support of Interprofessional Collaborative Education
- “After almost 50 years of inquiry, there is now sufficient evidence to indicate that interprofessional education enables effective collaborative practice which in turn optimizes health services, strengthens health systems, and improves health outcomes…research evidence has shown a number of results (including):
- Improve access to and coordination of health-services
- Improve appropriate use of specialist clinical resources
- Improve health outcomes for people with chronic diseases
- Improve patient care and safety
- Decrease total patient complications
- Decrease length of hospital stay
- Decrease tension and conflict among caregivers
- Decrease staff turnover
- Decrease hospital admissions (or readmissions)
- Decrease clinical error rates
- Decrease mortality rates
- “After almost 50 years of inquiry, there is now sufficient evidence to indicate that interprofessional education enables effective collaborative practice which in turn optimizes health services, strengthens health systems, and improves health outcomes…research evidence has shown a number of results (including):
- Additionally, research has shown that failures in communication are consistently one of the top three root causes of sentinel events. The National Academy of Medicine (formerly the IOM) has a series of reports demonstrating the relationship between poor team performance and negative patient outcomes and recommends implementation of IPCE as a solution.
- “Interprofessional teamwork and collaboration practice are emerging as key elements of efficient and productive work in promoting health and treating patients. The vision for these collaborations is one where different health and/or social professionals share a team identify and work closely together to solve problems and improve delivery of care.” Source: Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes. (National Academy of Medicine, 2015).
Supported Activity Types & Credit Types
- We support the following activity types:
- Live Courses including in-person, virtual, cohort, conference etc.
- Regularly Scheduled Series
- Enduring Material otherwise known as on-demand or asynchronous learning
- Journal- Based or journal clubs
- Performance Improvement including quality improvement or research-based
- We do NOT support Faculty Credit (or Learning from Teaching), Test-Item Writing, Internet Searching for Learning, or Manuscript Review
- We offer the following credit types:
- In support of improving patient care, Sutter Health, is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
- Through Joint Accreditation, Sutter Health is also able to provide Association of Social Work Boards (ASWB) credit to social workers at its activities.
- We offer the following Maintenance of Certification (MOCs) on some activities:
- American Board of Anesthesiology (ABA)
- American Board of Internal Medicine (ABIM)
- American Board of Otolaryngology- Head & Neck Surgery (ABOHNS)
- American Board of Pathology (ABPath)
- American Board of Pediatrics (ABP)
- American Board of Surgery (ABS)
- American Board of Orthopaedic Surgery (ABOS)- Coming soon!
- American Board of Thoracic Surgery (ABTS)- Coming soon!
- We support the following activity types:

Accreditation & Benefits of Partnering with CPD
(What is) Joint Accreditation
- A leading model for interprofessional collaborative practice, Joint Accreditation for Interprofessional Continuing Education establishes the standards for education providers to deliver IPCE planned by the healthcare team for the healthcare team.
- Joint Accreditation improves educational efficiency by integrating medical, nursing, pharmacy, and other healthcare discipline accredited continuing education criteria in a single, unified set of accreditation standards.
- For more information: https://www.jointaccreditation.org/glance
Joint Accreditation Criteria
- Planning Team Requirements: Joint Accreditation criteria require that Interprofessional Continuing Education activities are planned by and for the healthcare team. For activities that are focused on multiple professions, the planning team should reflect the professions and credit types being targeted by the activity.
- Educational Quality & Independence: Jointly accredited continuing education providers must meet rigorous standards for educational quality and independence – including the Standards for Integrity and Independence in Accredited Continuing Education and incorporation of evidence-based best practices in healthcare education. This ensures that healthcare teams receive education that is designed to be free from commercial bias or conflict of interest, based on valid content, and effective in improving the quality and safety of care delivered by the team.
- Additional Primary Criteria:
- The provider incorporates into IPCE activities the educational needs (knowledge, skills/strategy, or performance) that underlies the practice gaps of the healthcare team and/or the individual members’ knowledge, skills/strategy, or performance as members of the healthcare team.
- The provider generates activities/ educational interventions that are designed to change the skills/strategy or performance of the healthcare team and/or patient outcomes.
- The provider designs education that promotes active learning- so that teams learn from, with, and about each other- consistent with the desired results.
- The provider develops activities/ educational interventions in the context of desirable attributes of the healthcare team (e.g., ACCME or ABMS competencies; interprofessional team competencies: values/ ethics, roles, and responsibilities, interprofessional communication, teams, and teamwork).
- The provider utilizes support strategies to sustain change as an adjunct to its educational interventions (e.g., enabling and reinforcing strategies such as reminders, patient feedback).
- The provider implements strategies to remove, overcome, or address barriers to change in the skills/ strategy or performance of the healthcare teams.
- The provider analyzes changes in the healthcare team (skills/strategy, performance) and/or patient outcomes achieved as a result of its IPCE activities/ educational interventions.
- Commendation Criteria:
- The provider engages patients as planners and teachers in accredited IPCE and/or CE.
- The provider engages students of the health professions as planners and teachers in accredited IPCE and/or CE.
- The provider supports the continuous professional development of its own education team.
- The provider engages in research and scholarship related to accredited IPCE and/or CE and disseminates findings through presentation or publication.
- The provider integrates the use of health and/or practice data of its own learners in the planning and presentation of accredited IPCE and/or CE.
- The provider identifies and addresses factors beyond clinical care (e.g., social determinants) that affect the health of patients and integrates those factors into accredited IPCE and/or CE.
- The provider collaborates with other organizations to address population health issues.
- The provider designs accredited IPCE and/or CE (that includes direct observation and formative feedback) to optimize communication skills of learners.
- The provider designs accredited IPCE and/or CE (that includes direct observation and formative feedback) to optimize technical and procedural skills of learners.
- The provider creates and facilitates the implementation of individualized learning plans.
- The provider demonstrates the positive impact of its overall IPCE program on patients or their communities.
Benefits of Partnering with CPD
- Structure, Dedication, Reliability: CPD provides a work ethic focused solely on the tracking and documentation of skills, knowledge, and experience in the development (not simply training) of your professional workforce.
- Jointly Accreditation with Commendation provider which adheres to education quality standards necessary to promote safe and highly reliable health care. Partnering with us will help you position yourselves for the future of integrated care.
- Lower Cost & Higher Quality: Centralized CPD services eliminates redundant staffing & fees, facilitates organizational alignment on evidence-based practice, and allows coaching on innovative design.
- Greater integration with other education leaders from many disciplines across the organization. You stand to receive great insight & learning from integrating with like-minded professionals within the organization.
- Electronic outcomes analysis dashboard for measurement of performance metrics. We provide a dedicated, continuing education specific, Learner Management System.
- Planning & content recommendations to promote inclusion of Patient & Family Advisors, active learning paired with enabling & reinforcing strategies for sustainability, addressing practice gaps, competency development, implementation barriers & more!

 Facebook
Facebook Twitter
Twitter LinkedIn
LinkedIn Forward
Forward

